The 1st concussion consensus statement was published after the 2001 international Concussion in Sport group met in Vienna, and one of their findings was that neuropsychological testing was the cornerstone of concussion management.
(The Concussion in Sport group is an international panel of the leading researchers in the field of concussions. They have released 5 statements since 2001 that amalgamate the latest research and best practice recommendations.)
Since 2001 there has been proliforation of baseline testing methods from the various versions of the SCAT put forward by the Concussion in Sport group, to various pen and paper tests, and computerized tests. The one common goal is that they were put into place to create objective data to be utilized for post-concussion comparisons to help in management and recovery.
So a little disclaimer, I’m a physiotherapist involved in concussion management, which includes Baseline concussion testing (BCT) as part of our management. I direct the Concussion Solutions Program at Honsberger Physio+, and have been involved in concussion management for over 20 years.
In July 2017, Parachute Canada’s expert advisor concussion subcommittee released the Canadian Guidelines on Concussion in Sport. One of their key recommendations was that BCT of youth and adult recreation athletes using any tools or combination tools was not required to provide post-injury care of those who sustained suspected or diagnose concussion. Baseline testing was not recommended in youth athletes regardless of sport or level of play.
This has created some confusion in the world of baseline testing, just as more athletes were becoming familiar and proactive in concussion management.
These recommendations did not totally align with the most recent concussion consensus statement from the Concussion in Sport group from Berlin 2016. In the Berlin statement, they indicated that “baseline or preseason neuropsychological testing was considered by the panel and was not felt to be required as a mandatory aspect of every assessment; however it may be helpful or add useful information to the overall interpretation of these tests. It also provides an additional educational opportunities for the healthcare provider to discuss the significance of this injury with the athlete.”
As a physiotherapist, baseline concussion testing serves three key functions in my practice:
- Educate before a concussion injury happens to ensure the proper process is followed immediately from the moment a possible concussion suspected. Concussion education is also a key recommendation from Ontario’s Rowan’s Law that was passed in 2017 regarding concussion injuries.
- Provides a point of comparison in terms of neurocognitive status to assist in the post concussion management.
- Adds another layer of information regarding the recovering athlete with respect to their ability to return to learn and return to play. This information, in addition to a change in symptoms, family feedback and successful completion of progressive activity in the return to play stages provides a detailed awareness of an individual’s status.
If we take the educational process out of the Baseline concussion testing equation, why should an individual still have a baseline concussion test done? The majority of healthcare providers that treat individuals after concussion injury do find that having a baseline concussion score does allow for better management- safer, structured to meet the individuals neurocognitive needs, and provides an objective comparison throughout the overall recovery process. But according to the Parachute Canada guidelines a baseline test is not needed for proper management, so why still do it?
Several studies over the past three to four years have shown that even with proper medical clearance, current research does show that within the first year of return to play after concussion injury, athletes have a 2-4 times increase risk in developing musculoskeletal injuries.
Studies evaluating professional soccer, Australian football, as well as collegiate Sports such as football, basketball, soccer and lacrosse all noted this evidence with a peak musculoskeletal injury levels within the first 3 months after return to play. This trend has been seen up to one year after return-to-play was also seen up to 2 years post injury in a military specific study.
Various researchers have postulated theories for this increase musculoskeletal injury risk such as:
- decreased cardiovascular fitness
- decreased neural cognitive ability
- unresolved neuromuscular impairments
- delayed reaction times
- short-term brain changes
- decreased psychological “readiness”
- altered trunk movement patterns
- lower extremity stiffness
- gait changes
Studies have shown that after symptom resolution, there lingering effects in postural control, gait sequencing and dynamic balance. These effects can affect neuromuscular control and most notable during physically and cognitively challenging athletic activities.
It has been found that deficits from concussion injury may last longer than reported and may be present even after the return to unrestricted activity suggesting that current clinical assessment tools may lack sufficient sensitivity to accurately track functional recovery.
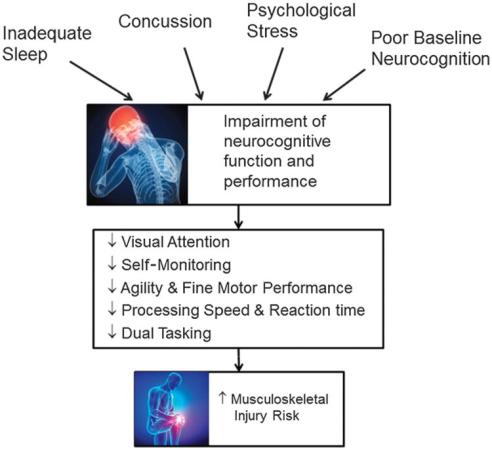
One of the main areas that has been evaluated is that of neurocognitive abilities. Neurocognitive performance encompasses the domains of visual attention, self-monitoring, agility, fine motor performance, processing speed, reaction time, and dual tasking ability. Neurocognitive performance is often a key measure in baseline concussion testing.
After concussion injury there are short-term changes in reaction time, visuospatial awareness, attention, executive decision making, and movement coordination. Any deficits in these areas can result in a decrease overall neurocognitive performance.
The presence of an increase risk of a subsequent musculoskeletal injury after concussion, as well as lingering effects in postural control, gait sequencing, and dynamic balance, leads to the speculation that current return-to-play protocol are not effective for ensuring a safe return to play for the athlete as a whole versus focused on being “brain” safe only.
Although some current concussion guidelines call into question the use of concussion Baseline testing, the ability to create baseline neurocognitive scores in the pre-injury state is valuable. This allows for a neurocognitive comparison post-injury, to ensure an athlete to has returned to normal neurocognitive levels to minimize the risk of musculoskeletal injuries, or other lingering post-concussion neuromuscular issues. Based on the scores post-injury, a health care provider can better determine whether an athlete is ready to return to play for all health states.
As the data continues to show, recovery from a concussion can be more prolonged than the standard post concussion symptoms demonstrate. Ensuring that an individual has returned to their pre-concussion neurocognitive levels via training and post-injury testing allows for a safer return with a minimized risk of prolonged issues. Ensuring a full neurocognitive recovery via an extra step of neurocognitive training is key.
Although the rationale for baseline concussion is contradictory based on the current concussion guidelines, the BCT process can be used for athlete education, planning of post injury recovery, and also ensuring a full return to pre injury neurocognitive levels to minimize musculoskeletal injury risk.

 At Honsberger Physio+, the use of components including the Dynavision D2, Neurotracker, fitLight and PlayAttention has been shown to increase neurocognitive performance in a variety of sports across a wide spectrum of ages. Honsberger Physio+ has 2 state of the art Vision Performance Centres, which are dedicated to sports vision, athlete development, concussion testing and recovery, and for anyone wanting to perform at their best! They are one of the only facility in Canada to combine these 5 pieces of technology focused on reaction time, peripheral vision, depth perception and neuroplasticity. The only other institution in Canada to have the 3D FitLight wall is the Toronto Raptors.
At Honsberger Physio+, the use of components including the Dynavision D2, Neurotracker, fitLight and PlayAttention has been shown to increase neurocognitive performance in a variety of sports across a wide spectrum of ages. Honsberger Physio+ has 2 state of the art Vision Performance Centres, which are dedicated to sports vision, athlete development, concussion testing and recovery, and for anyone wanting to perform at their best! They are one of the only facility in Canada to combine these 5 pieces of technology focused on reaction time, peripheral vision, depth perception and neuroplasticity. The only other institution in Canada to have the 3D FitLight wall is the Toronto Raptors.
